GENERAL MEDICINE ASSIGNMENT FOR MAY 2021
- Get link
- X
- Other Apps
I have been given the following cases to solve in an attmept to understand the topic of 'Patient clinical data analysis' to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and diagnosis and coem up with a treatment plan.
Below are my answers to the Medicine Assignment based on my comprehension of the cases.
20 YEARS BACK -- first episode of SOB
15 YEARS BACK -- facial puffiness
12 YEARS BACK --second episode of SOB
yearly episodes from the past 12 years
8 YEARS BACK -- diagnosed with diabetes
5 YEARS BACK -- anemia and took Fe injections
1 MONTH BACK-- Genrealized weakness
15 DAYS BACK-- Pedal edema
ANATOMICAL LOCALIZATION ---
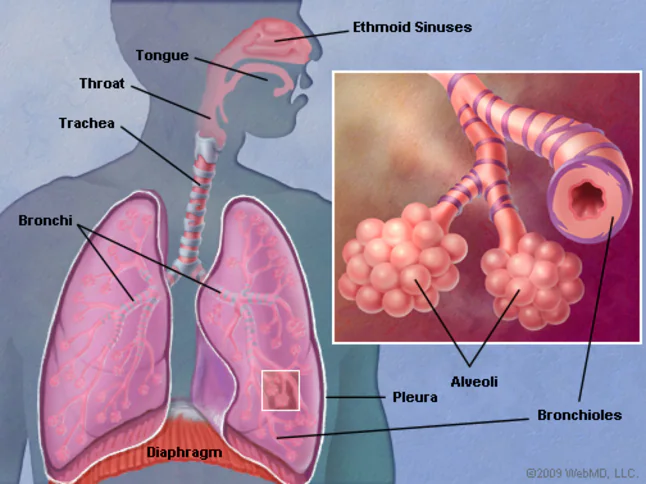
LUNGS-Bronchi and bronchioles -
CASE 2 : https://143vibhahegde.
Q1 What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
HIPPOCAMPUS
FRONTAL LOBE
ETIOLOGY:
CHRONIC ALCOHOLISM
Research into the neurobiology of responsiveness to placebo has addressed placebo analgesia; accordingly, the neurobiology of placebo effects is commonly considered in terms of opioid and non-opioid mechanisms.[9,10] Several studies have demonstrated that placebo effects can be completely or partially reversed by the opioid antagonist naloxone, supporting the involvement of endogenous opioids in some analgesic effects of placebo.[11–14] Furthermore, analgesic effects of placebo are likely to be inhibited by the peptide cholecystokinin (CCK) for they are potentiated when a CCK antagonist is administered. Considered together, these studies de,16]
INDICATIONS:
PAIN
INSOMNIA
ANXIETY
RISK OF SUBSTANCE ABUSE
EFFICACY:
The efficacy of placebo was clear, and varied not only between the five indication groups but also within them. Whereas placebo, unlike active treatment, produced hardly any improvement in symptoms in patients with severe stroke, it was as effective as active treatment in patients with mild neurological deficits, producing an improvement of about 50%. In patients with angina pectoris, placebo produced an increase in exercise tolerance (treadmill walking time to onset of ST-segment depression and angina attacks) of about 10% on average, compared with about 22% under active treatment (nisoldipine). In diabetes therapy, placebo produced no improvement in fasting and postprandial blood glucose levels compared with active treatment (acarbose), and also had no effect on HbA1C values.
USEFULLNESS:
The use of placebo is not equivalent to the absence of treatment, for example, placebo could be used in addition to standard care. In all cases, its use should be associated with measures to minimize exposure and avoid irreversible harm, especially in serious or rapidly evolving diseases. As appropriate, rescue treatment and escape procedures should be set up.
Other situations where the use of placebo should be scrutinized and challenged include run-in periods where a protocol requires active treatment to be withheld.
Situations in which placebo may be considered as a comparator, for example, might be when there is no commonly accepted therapy for the condition and the investigational medicinal product is the first one that may modify the course of the disease process.
It is useful when the commonly used therapy for the condition is of questionable efficacy or carries with it a high frequency of undesirable adverse reactions and the risks may be significantly greater than the benefits.[24]
3) Why have neurological symptoms appeared this time, that were absent during withdrawal earlier? What could be a possible cause for this?
KINDLING ALCOHOL WITHDRAWL
4) What is the reason for giving thiamine in this patient?
This was associated with Bilateral Hearing loss, aural fullness and presence of tinnitus.
- He has associated vomiting- 2-3 episodes per day, non projectile, non bilious containing food particles.
- Patient has H/o postural instability- he is unable to walk without presence of supports, swaying is present and he has tendency to fall while walking
- No diplopia, dysphagia, dysarthria
- No H/o any seizure like activity.
ANATOMICAL LOCALIZATION:
THERE IS PRESENCE OF AN INFART IN INFERIOR CEREBELLAR HEMISPHERE OF BRAIN
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
- GASTROENTEROLOGY( & PULMONOLOGY)
- CASE-1: https://63konakanchihyndavi.
blogspot.com/2021/05/case- discussion-on-pancreatitis- with.html - Q1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
- A1) Timespan of symptomology:
- 5 years ago: 1st episode of pain abdomen and vomiting
- 1 year back: 5 to 6 episodes of pain abdomen and vomiting
- 20 days back: Increased consumption of toddy intake
- Since 1 week: Pain abdomen and vomiting
- Since 4 weeks: Fever, constipation and burning micturition
- Anatomical localization: Pancreas and left lung
- Etiology: The pathophysiology of acute pancreatitis is characterized by a loss of intracellular and extracellular compartmentation, by an obstruction of pancreatic secretory transport and by an activation of pancreatic enzymes attributed to alcohol.
- Q2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
- A2) Inj. Metrogyl: Metronidazole is of the nitroimidazole class. It inhibits nucleic acid synthesis by forming nitroso radicals, which disrupt the DNA of microbial cells.
- Inj. Meropenam: Meropenem is bactericidal except against Listeria monocytogenes, where it is bacteriostatic. It inhibits bacterial cell wall synthesis like other β-lactam antibiotics. In contrast to other beta-lactams, it is highly resistant to degradation by β-lactamases or cephalosporinases.
- Inj. Amikacin: The primary mechanism of action of amikacin is the same as that for all aminoglycosides. It binds to bacterial 30S ribosomal subunits and interferes with mRNA binding and tRNA acceptor sites, interfering with bacterial growth.
- TOTAL PARENTAL NUTRITION
- Inj. Octerotide: Octreotide suppresses secretion of growth hormone (GH), and in many cases suppresses insulin-like growth hormone-1 (IGF-1) (somatomedin C). Sandostatin works centrally at the site of the tumor and binds to somatostatin receptors to regulate GH secretion and cell growth.
- Inj. Pantop: The mechanism of action of pantoprazole is to inhibit the final step in gastric acid production. In the gastric parietal cell of the stomach, pantoprazole covalently binds to the H+/K+ ATP pump to inhibit gastric acid and basal acid secretion.
- Inj. Thiamine: Mechanism of Action: Thiamine combines with adenosine triphosphate (ATP) in the liver, kidneys, and leukocytes to produce thiamine diphosphate. Thiamine diphosphate acts as a coenzyme in carbohydrate metabolism, in transketolation reactions, and in the utilization of hexose in the hexose-monophosphate shunt.
- Inj. Tramadol: Tramadol is a centrally acting analgesic with a multimode of action. It acts on serotonergic and noradrenergic nociception, while its metabolite O-desmethyltramadol acts on the µ-opioid receptor. Its analgesic potency is claimed to be about one tenth that of morphine.
- CASE-2: https://nehae-logs.blogspot.
com/2021/05/case-discussion- on-25-year-old-male.html - Q1) What is causing the patient's dyspnea? How is it related to pancreatitis?
- A1) Pleural effusion might be the cause of patients dyspnea.
- Presence of pleural effusion is currently considered an indication of severe pancreatitis and not just a marker of the disease[24]. Pancreatic ascites and pleural effusion are rare complications of both chronic and acute pancreatitis, and are associated with a mortality rate of 20% to 30%.
- Q2) Name possible reasons why the patient has developed a state of hyperglycemia.
- A2) Hyperglucagonemia secondary to stress could be the result of patient developing hyperglycemia.
- Elevated levels of catecholamines and cortisol.
- Q3) What is the reason for his elevated LFTs? Is there a specific marker for Alcoholic Fatty Liver disease?
- A3) Elevated liver enzymes are a sign that a person has an inflamed or a damaged liver. Many conditions may cause liver inflammation or damage. In this case the probable reason may be due to liver injury. Alanine aminotransferace (ALT) and Asparate aminotransferase (AST) are the specific markers for alcoholic fatty liver disease. Glutamyl transpeptidase (GGT) is another marker of liver injury, and this enzyme is elevated in people who consumes alcohol. Of all the enzyme markers GGT is the most sensitive biomarker of alcohol consumption.
- Q4) What is the line of treatment in this patient?
- A4) IVF: 125 ml/hr
- Inj. PAN 40mg i.v.
- Inj Zofer 4mg i.v.
- Inj. Tramadol 1amp in 100ml i.v.
- Tab. Dolo 650mg
- GRBS charting 6th hourly
- BP charting 8th hourly.
- CASE-3: https://chennabhavana.
blogspot.com/2021/05/general- medicine-case-discussion-1. html - Q1) What is the most probable diagnosis in this patient?
- A1) Abdominal Hemorrhage may be the most probable diagnosis in this patient.
- Q2) What was the cause of her death?
- A2) Cause of her death may be due to complications of laparotomy surgery such as hemorrhage, infection, or damage to internl organs
- .
- Q3) Does her NSAID abuse have something to do with her condition? How?
- A3) NSAIDS are known to cause drug induced hepatitis which may lead to cirrhosis.
- NEPHROLOGY ( AND UROLOGY)
- Q1) What could be the reason for his SOB ?
- A1) His shortness of breath may be due to Acidodsis which was caused by diuretics.
- Q2) Why does he have intermittent episodes of drowsiness ?
- A2) Hyponatremia was the cause for drowsiness.
- Q3) Why did he complaint of fleshy mass like passage in his urine?
- A3) Pyuria (Many pus cells) are passed in the urine which he observed as fleshy mass like passage.
- Q4) What are the complications of TURP that he may have had?
- A4) Bladder injury.
- Bleeding.
- Blood in the urine after surgery.
- Electrolyte abnormalities.
- Infection.
- Loss of erections.
- Painful or difficult urination.
- CASE-2:https://drsaranyaroshni.
blogspot.com/2021/05/an-eight- year-old-with-frequent.html
the fungus enters the sinuses from the environment and then the brain.
- Get link
- X
- Other Apps